Allergy 金黃色葡萄球菌引起表皮脂質(zhì)組成異常和皮膚屏障功能障礙
發(fā)布日期:2023-05-29
原標(biāo)題:金黃色葡萄球菌引起表皮脂質(zhì)組成異常和皮膚屏障功能障礙
——浙大迪迅 譯
背景:已知金黃色葡萄球菌定植會(huì)導(dǎo)致特應(yīng)性皮炎(AD)患者的皮膚屏障破壞。然而,金黃色葡萄球菌如何誘導(dǎo)異常的表皮脂質(zhì)組成和皮膚屏障功能障礙尚未得到研究。
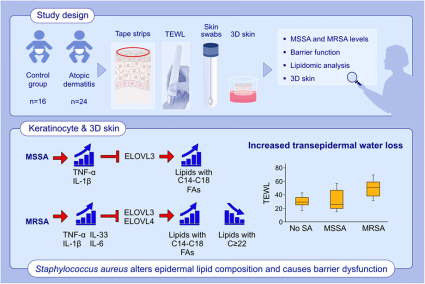
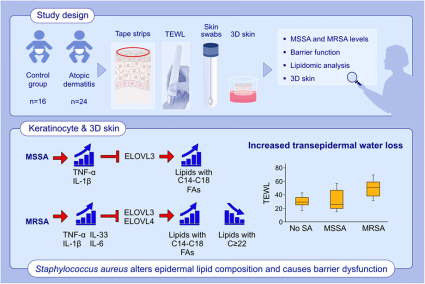
方法:從24名AD患兒(6.0±4.4歲)和16名健康兒童(7.0±4.5歲)獲得皮膚膠帶(STS)和拭子。STS樣品的脂質(zhì)組學(xué)分析通過(guò)質(zhì)譜法進(jìn)行。評(píng)估了對(duì)甲氧西林敏感菌和耐甲氧西林金黃色葡萄球菌(MSSA和MRSA)的皮膚水平。在原代人角質(zhì)形成細(xì)胞(HEKs)和器官型皮膚培養(yǎng)物中評(píng)估MSSA和MRSA的作用。
結(jié)果:經(jīng)MRSA定植的AD和器官型皮膚顯著增加脂質(zhì)種類(lèi)與非羥基脂肪酸鞘氨醇神經(jīng)酰胺與棕櫚酸的比例([N-16:0NS-CER]、鞘磷脂[16:0-18:0 SM])和溶血磷脂酰膽堿[16:0-18:0 LPC],但與沒(méi)有金黃色葡萄球菌定植的皮膚相比,顯著降低了相應(yīng)的超長(zhǎng)鏈脂肪酸(VLCFAs)物種(C22-28)的比例。在MRSA定植的AD皮膚中發(fā)現(xiàn)經(jīng)表皮失水(TEWL)顯著增加。金黃色葡萄球菌間接通過(guò)白細(xì)胞介素(IL)-1β,腫瘤壞死因子(TNF)-α,IL-6和IL-33抑制脂肪酸伸長(zhǎng)酶(ELOVL3和ELOVL4)在HEK中的表達(dá)。MRSA對(duì)ELOVL的抑制更為明顯,并導(dǎo)致器官型皮膚中的TEWL增加。對(duì)泛變應(yīng)原、母親 PFAS 和哮喘的 IgE 可能是 PFAS 相關(guān)的特征。
結(jié)論:異常的皮膚脂質(zhì)譜和屏障功能障礙與AD患者的金黃色葡萄球菌定植有關(guān)。這些影響歸因于金黃色葡萄球菌誘導(dǎo)的 IL-1β、TNF-α、IL-6 和 IL-33 在角質(zhì)形成細(xì)胞模型中對(duì) ELOVL 的抑制,并且在 MRSA 中比 MSSA 更突出。
原始出處
Allergy
DOI: 10.1111/all.15640
Abstract:
Background: Staphylococcus (S) aureus colonization is known to cause skin barrier disruption in atopic dermatitis (AD) patients. However, it has not been studied how S. aureus induces aberrant epidermal lipid composition and skin barrier dysfunction.
Methods: Skin tape strips (STS) and swabs were obtained from 24 children with AD (6.0?±?4.4?years) and 16 healthy children (7.0?±?4.5?years). Lipidomic analysis of STS samples was performed by mass spectrometry. Skin levels of methicillin-sensitive and methicillin-resistant S. aureus (MSSA and MRSA) were evaluated. The effects of MSSA and MRSA were evaluated in primary human keratinocytes (HEKs) and organotypic skin cultures.
Results: AD and organotypic skin colonized with MRSA significantly increased the proportion of lipid species with nonhydroxy fatty acid sphingosine ceramide with palmitic acid ([N-16:0 NS-CER], sphingomyelins [16:0–18:0 SM]), and lysophosphatidylcholines [16:0–18:0 LPC], but significantly reduced the proportion of corresponding very long-chain fatty acids (VLCFAs) species (C22–28) compared to the skin without S. aureus colonization. Significantly increased transepidermal water loss (TEWL) was found in MRSA-colonized AD skin. S. aureus indirectly through interleukin (IL)-1β, tumor necrosis factor (TNF)-α, IL-6, and IL-33 inhibited expression of fatty acid elongase enzymes (ELOVL3 and ELOVL4) in HEKs. ELOVL inhibition was more pronounced by MRSA and resulted in TEWL increase in organotypic skin.
Conclusion: Aberrant skin lipid profiles and barrier dysfunction are associated with S. aureus colonization in AD patients. These effects are attributed to the inhibition of ELOVLs by S. aureus-induced IL-1β, TNF-α, IL-6, and IL-33 seen in keratinocyte models and are more prominent in MRSA than MSSA.
First Author:
Jihyun Kim
Correspondence Author:
Elena Goleva
Correspondence:
Department of Pediatrics, National Jewish Health, 1400 Jackson St, Denver, CO 80206, USA.
Email: golevae@njhealth.org
原始出處
Allergy
[IF:13.146]
Staphylococcus aureus causes aberrant epidermal lipid composition and skin barrier dysfunctionDOI: 10.1111/all.15640
Abstract:
Background: Staphylococcus (S) aureus colonization is known to cause skin barrier disruption in atopic dermatitis (AD) patients. However, it has not been studied how S. aureus induces aberrant epidermal lipid composition and skin barrier dysfunction.
Methods: Skin tape strips (STS) and swabs were obtained from 24 children with AD (6.0?±?4.4?years) and 16 healthy children (7.0?±?4.5?years). Lipidomic analysis of STS samples was performed by mass spectrometry. Skin levels of methicillin-sensitive and methicillin-resistant S. aureus (MSSA and MRSA) were evaluated. The effects of MSSA and MRSA were evaluated in primary human keratinocytes (HEKs) and organotypic skin cultures.
Results: AD and organotypic skin colonized with MRSA significantly increased the proportion of lipid species with nonhydroxy fatty acid sphingosine ceramide with palmitic acid ([N-16:0 NS-CER], sphingomyelins [16:0–18:0 SM]), and lysophosphatidylcholines [16:0–18:0 LPC], but significantly reduced the proportion of corresponding very long-chain fatty acids (VLCFAs) species (C22–28) compared to the skin without S. aureus colonization. Significantly increased transepidermal water loss (TEWL) was found in MRSA-colonized AD skin. S. aureus indirectly through interleukin (IL)-1β, tumor necrosis factor (TNF)-α, IL-6, and IL-33 inhibited expression of fatty acid elongase enzymes (ELOVL3 and ELOVL4) in HEKs. ELOVL inhibition was more pronounced by MRSA and resulted in TEWL increase in organotypic skin.
Conclusion: Aberrant skin lipid profiles and barrier dysfunction are associated with S. aureus colonization in AD patients. These effects are attributed to the inhibition of ELOVLs by S. aureus-induced IL-1β, TNF-α, IL-6, and IL-33 seen in keratinocyte models and are more prominent in MRSA than MSSA.
First Author:
Jihyun Kim
Correspondence Author:
Elena Goleva
Correspondence:
Department of Pediatrics, National Jewish Health, 1400 Jackson St, Denver, CO 80206, USA.
Email: golevae@njhealth.org
 杭州浙大迪迅生物基因工程有限公司
杭州浙大迪迅生物基因工程有限公司

